Removing the Picture-Perfect Lens on the Reality of Postpartum Depression
Life on social media with a new baby may look—literally—picture perfect. Instagram and Facebook fields highlight all the excitement and thrilling moments. Maybe you’re seeing beautifully lit pictures of smiling families, babies in perfectly clean outlets, and new moms with perfect hair and freshly painted fingernails.
However, that portrayal is not the reality for new or even experienced moms, especially for women experiencing postpartum depression (PPD).
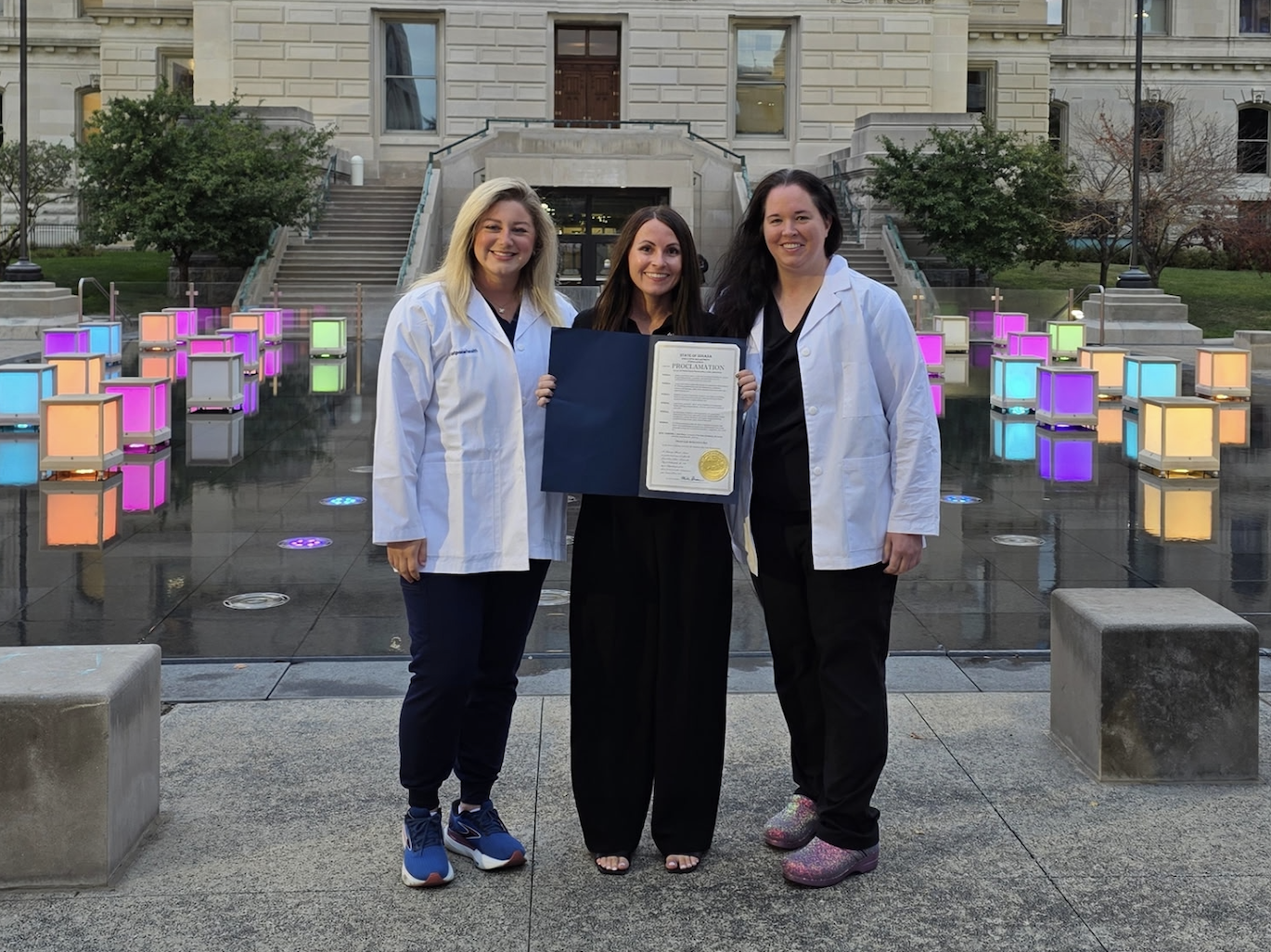
“It’s not always a fairytale and a perfect time, and that’s okay,” says Nikita Duke, DNP, PMHNP-BC, psychiatric mental health practitioner and Director of Behavioral Health at Fast Pace Health.
While postpartum depression happens more than many realize, an unrealistic stigma still exists that a mom is weak or a “bad” mom for seeking help when she knows things aren’t right.
“Not seeking help can put a strain on the relationship between the mom and the baby,” says Duke.
Expecting Perfection
There is no “typical” or standard motherhood. However, women may have a perfect idea about motherhood. Even Duke experienced this.
When Duke’s twins, who are now 7, were born, doctors suddenly moved the date of her planned C-section. So, while her twin daughter was healthy at birth, her twin son had to spend two weeks in the NICU.
She recalls feeling helpless in the situation and did all she could do, which often included sudden tears at times and even feeling terrified when her son joined their family at home.
“When he cried, I was worried his lungs still weren’t ready and something could happen again,” she shares.
While Duke experienced acute stress, not postpartum depression, she knows the line between the two is not fair, and PPD can even happen to healthcare providers.
Beyond the Baby Blues
The birth of a baby can bring up overwhelming emotions. New mothers can experience anything from joy to fear. However, it can also result in something unexpected – depression.
Every mother, according to Duke, may experience the “Baby Blues.” The term refers to a period 3-5 days after birth where hormones suddenly change. During this time, mothers may experience mood swings, sudden crying, anxiety, and difficulty sleeping.
These hormonal changes and the added pressure of caring for a new life can cause significant stress to women. Usually, after the first week, the woman will feel more like herself, and these initial major anxieties will fade.
Sometimes postpartum depression can be mistaken for baby blues at first. However, if the signs of depression and anxiety last longer than two weeks or interfere with the ability to care for yourself or your baby, it may be a sign of a more serious issue. Signs to look for include: feeling your baby is a hassle, a lack of attachment with the baby, feelings of regret, loss of motivation in general, and even distancing from friends and family. This could mean the woman could have postpartum depression.
Some women are at a higher risk, as well, says Duke. In addition, things like a previous PPD diagnosis, predisposition or family tendency toward depression, and the environment and support system can also add to the postpartum depression experience.
Addressing Concerns
Healthcare providers can address and help treat postpartum depression. The key, Duke says, is early intervention.
You should feel free to address any mental health concerns at your follow-up appointments or see your provider for a mental health-specific appointment. Duke reminds moms to answer any screening questions honestly with healthcare providers to have all the information to help support the mom.
From there, your practitioner may treat the patient directly or find outside resources. Resources include medications, coping strategies, and appointments with specialized healthcare providers.
Duke knows one concern mothers have about seeking help and medicine is the safety of using medications while breastfeeding. So, Duke has discussed the risks and benefits of medication with her patients and their OBGYNs for input on medications.
A mother may fear that an initial PPD diagnosis may stay with them forever. However, even when resources are put in place, such as medication or counseling, they don’t necessarily need to continue forever. It is just what is needed at that moment under the direction of your healthcare providers and the progress of the patient.
When to See a Provider
Mothers may feel embarrassed if they’re depressed or anxious after a baby’s birth. However, if you’re experiencing any symptoms of postpartum depression, it’s important to seek treatment as early as possible.
Call your OBGYN, local practitioner, or stop by our clinics if you experience the following symptoms or if they get worse after two weeks:
- Difficulty caring for your baby
- Difficulty completing everyday tasks
- Worsening depression and/or anxiety
Fast Pace Health also offers telehealth appointments to discuss postpartum depression. A telehealth appointment means one doesn’t even have to leave the house, carry the baby or arrange for childcare. Telehealth services can also be used to meet with a counselor or therapist.
If you are ready to discuss your postpartum depression concerns or experience, find a clinic near you or find more information on our website.
–
This article was originally published Oct. 8, 2021.
Related Resources