Are You “Antibiotics Aware”?
You’re likely familiar with the phrase “too much of a good thing,” and that adage applies to one aspect of medicine today.
While antibiotics have saved lives over the years, they tend to be overprescribed or inappropriately prescribed. In this case, they can create a host of nasty side effects. Think nausea, vomiting, diarrhea and super-imposed secondary infections and at the extreme, infections are resistant to a large number of antibiotics. The latter can cause infections that resist healing resulting in advanced illness or even death.
A Cause for Alarm
According to the CDC, consider the fact that in 2014, 266.1 million courses of antibiotics were dispensed to outpatients in U.S. community pharmacies. This equates to more than 5 prescriptions written each year for every 6 people in the United States. Worse yet, at least 28% of antibiotics prescribed in the outpatient setting are unnecessary, meaning that no antibiotic was needed at all.
You might be thinking that this sounds serious — and it’s something healthcare providers are doing their best to address. Antibiotic Stewardship is a best practice movement that entities like Fast Pace Health have embraced for the good of the patient and the community at large.
Taking a Stand
Though not a new concept, more and more healthcare institutions are signing on to the idea of acting more responsibly in the context of issuing prescriptions. The goal is always patient safety first, thus maximizing the benefit of antibiotics and minimize harm to individuals and communities. Healthcare providers and their organizations committed to Antibiotic Stewardship agree to implement interventions to achieve this goal and track progress over time. In turn, patients can benefit from the peace of mind of knowing their risk of adverse reactions as well as the risk of contracting secondary infections is reduced and controlled.
‘Do No Harm’
Fast Pace Health is among those in the healthcare space leading the charge in this mission. Hear as Dr. Sarika Aggarwal, Chief Medical Officer at Fast Pace Health, translates Antibiotic Stewardship into action. “As we approach US Antibiotic Awareness Week November 18-24, 2022, the Office of Medical Affairs at Fast Pace Health in our continued commitment to patients is launching an ‘Antibiotic Stewardship program’. Our goal is to help our providers appropriately prescribe antibiotics using evidence-based guidelines, thus protecting our patients from the adverse effects of antibiotics and antibiotic resistance. An equally important goal is to educate our patients enabling them to participate in shared decision-making with their providers on the appropriate role of antibiotics for their infections.”
With the focus on positive outcomes for patients, Dr. Simon Spilkin, Medical Director at Fast Pace Health, adds, “The purpose of any antimicrobial stewardship program is to decrease antibiotic resistance and improve patient safety and outcomes. The Office of Medical Affairs at Fast Pace Health will achieve this goal through the commitment of all of our medical providers. The main interventions employed will include a combination of evidence-based protocols for common acute illnesses to guide our providers and educational materials in the form of electronic and print media for our patients. We hope through this partnership with the communities we serve that we can make a measurable impact on the appropriate prescription of antibiotics.”
Fast Pace Health providers are already on board with the new Antibiotic Stewardship Program. “As a Fast Pace provider, I am proud to make the commitment to serve my community by following safety guidelines for appropriate prescribing of antibiotics. It is my duty and honor to work with my patients to form an appropriate care plan that both meets their needs and does no harm. Our patients deserve the best care possible, and that is exactly what Fast Pace providers aim to provide”, said Chelsa Frey, MSN, FNP-C at Fast Pace Health.
Staying Informed
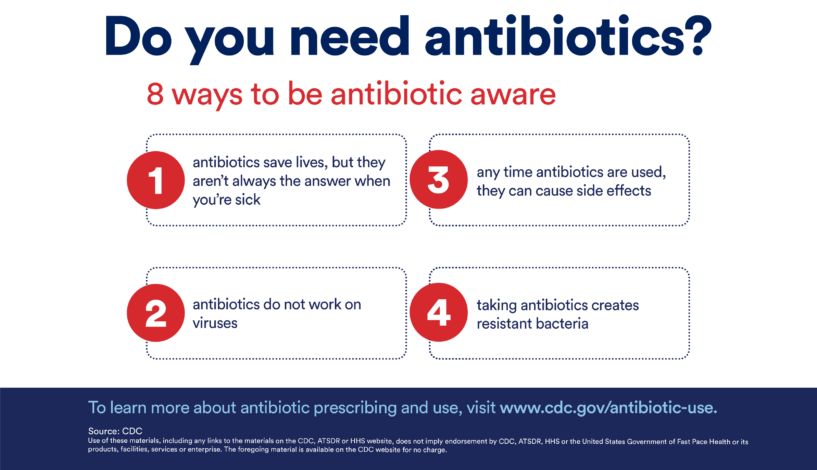
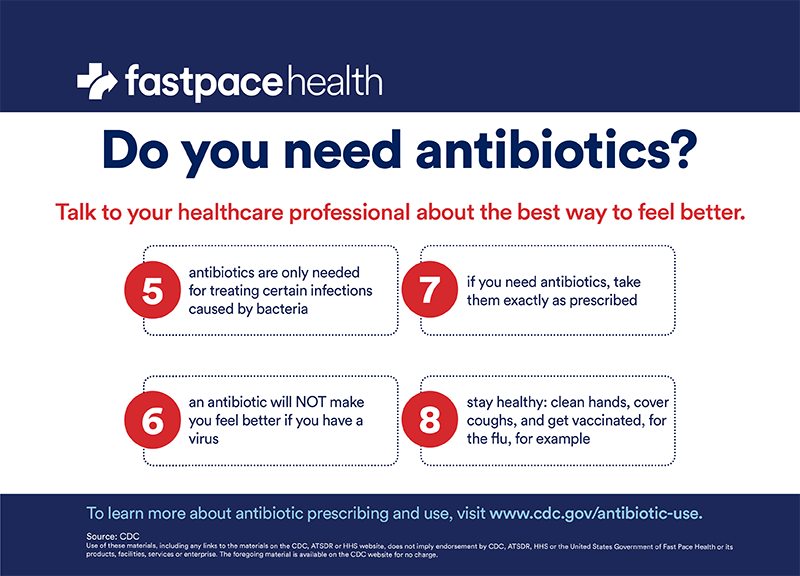
You might be wondering how to advocate for yourself and your family when it comes to antibiotic resistance and appropriate prescribing and uses for common infections. Your provider should listen carefully to evaluate your symptoms and medical history and only prescribe antibiotics if they’re truly necessary. It’s your right as a patient to ask questions and speak up if you feel the risks outweigh the potential benefits. You can also visit the CDC’s site to learn more about how to be “antibiotics aware.”
Related Resources


